Reconstructive plastic surgery through Relimb – what can they do for you?

Relimb is the UK’s first, private, surgical service dedicated to the treatment of patients who have suffered from traumatic injury, including amputation. Here, co-founder Norbert Kang talks us through what’s so special about what they do.
Setup by two plastic surgeons in 2018, Relimb has drawn together a group of professionals dedicated to providing world-class care for patients who often suffer from having injuries that cannot be treated by a single, traditional practitioner. The team includes clinical psychology, prosthetics and specialist physiotherapy, microbiologists, and anaesthetists who are experts in the pain experienced by amputees and those suffering from catastrophic injury.
Founders Norbert Kang and Alex Woollard are consultant plastic surgeons with over a decade of experience in complex reconstruction. This, coupled with their experience in osseointegration (over 50 cases) and nerve surgery (one of the largest series of targeted muscle reinnervation in Europe) allows Relimb to offer a service that is unique in both the UK, but even worldwide. Relimb can provide bespoke solutions for patients with complex bony and soft tissue polytrauma. Relimb has created a “one-stop-shop” through which a patient can access all the reconstructive options they may need, together with the support services that are required to achieve a successful outcome. In the table below, we list just a few of the types of treatments that we offer.
-
Reconstruction
Stump refashioning and scar revision; bone, soft-tissue, and nerve of the upper and lower limbs; soft-tissue including external genitalia, breast, abdominal wall, perineum.
-
Osseointegration
Upper and lower limb and after craniofacial injury or loss for fixation of a prosthetic eye, nose, and ear.
-
Nerve surgery
Regenerative peripheral nerve interface (RPNI); Targeted Muscle Reinnervation (TMR). Facial nerve injuries.
-
Complex hand problems
For example after combined injury to bone, tendon, nerve, soft-tissue.
-
Neuroma and Phantom Limb Pain
Surgical and non-surgical treatment.
-
All types of scar management
Neuromas, reduce the size of the scarred areas and hypertrophic and keloid scars.
-
Surgical treatment of brachial plexus injury
To relieve pain and restore sensation and motor function to your shoulder, arm, and hand.
-
Clinical Psychology support
Ensuring positive outcomes after treatment in both health and emotional well-being.
Finding the right solution after limb loss
Form strongly follows function and vice versa. If it looks right, it probably works right too. That goal becomes harder and harder to achieve as the starting point for our interventions deviates more and more from normality, in fact the starting point is as far as you can get from normality after an amputation or loss of/damage to other body parts. Nevertheless, Relimb is equipped to deal with the majority of both the smallest and largest of reconstructive problems, affecting any part of the human body.
To illustrate the scope of work undertaken by Relimb, we will describe three cases treated by the service over the last 4 years.
Case 1 –
This patient was involved in an industrial accident in 2019 in which their right ear was avulsed together with their entire scalp. To restore form, the patient elected to have their missing ear replaced with a silicone prosthesis held in place with osseointegrated bone-anchors placed into the temporal bone. Surgery was carried out in two stages, two months apart. The photographs below illustrate the progress of the patient through each stage of the process from start to finish.

Case 2 –
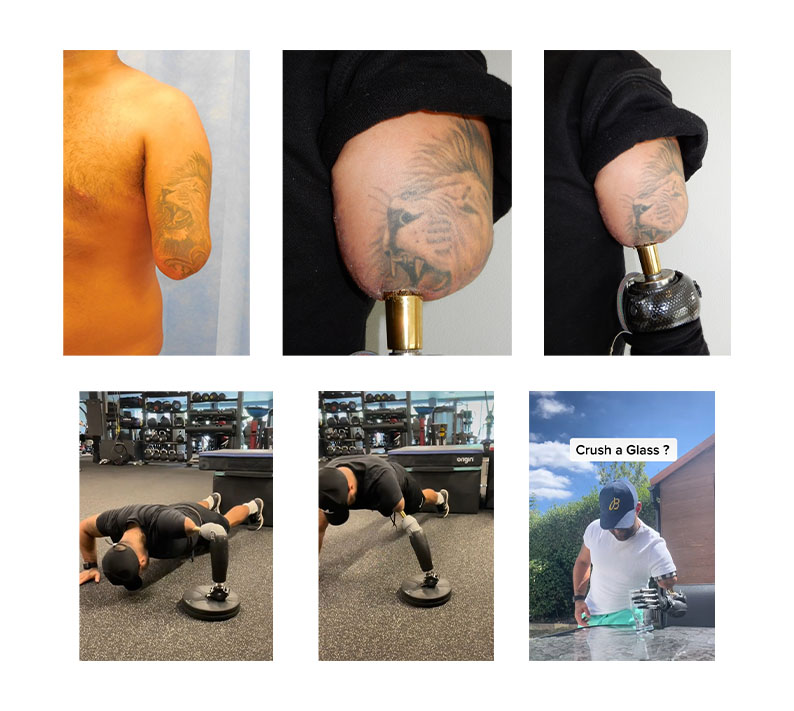
This patient was involved in a train accident in 2016 in which their left arm was traumatically amputated above the elbow.
There are two options for replacing an absent arm. The first is an allograft limb transplant (taking a limb from a living, but brain-deceased donor). The second is to use a prosthetic replacement.
Allograft limb transplantation is not technically difficult but obtaining a matching limb (i.e. exact colour match, length, appearance etc..) is impossible, donors are difficult to find and the technology for safe immunosuppression remains complicated and fraught with many long-term problems including permanent kidney and liver damage as well as increases in the risk of systemic infection and skin or other cancers. Moreover, the functional recovery of a transplanted limb after above elbow amputation is no different from that which can be achieved after a prosthetic reconstruction.
Therefore, prosthetic reconstruction forms the mainstay of reconstruction after limb loss. In this case, the patient opted for prosthetic reconstruction and never considered allograft transplantation.
However, he also decided that he wanted to maximise his functional recovery by undergoing two additional surgical procedures.
The first was to insert an osseointegrated implant (OI) into the residual humerus. The second was to undergo targeted muscle reinnervation (TMR) surgery. The aim of OI is to improve the way in which a patient can attach a prosthetic limb which makes it easier for them to gain the maximum return of function from their residual joints (in this case the shoulder) without compromising the function of the prosthesis.
The aim of the second procedure is to enhance the ability of the individual to regain control over the prosthetic limb so that it becomes functionally more useful. The photographs show the patient before and three years after surgery.
Case 3 –
This patient suffered from a right above knee amputation after being struck by a car while walking on the pavement.
Initially, they tried to manage to rehabilitate and mobilise with a socket-fitted prosthesis. However, it quickly became apparent that the socket was limiting the range of motion of the hip joint, and she was also suffering from constant pain in the stump due to rubbing and chaffing of the soft tissues.
Therefore, a decision was made to undergo treatment with an osseointegrated implant to simplify attachment of the prosthetic limb. Simultaneously, she underwent a targeted muscle reinnervation procedure to deal with symptoms of phantom limb pain. The photographs show the patient before and 8 months after surgery.

Surgery after limb loss
So far in this article, we have mentioned two key options for patients undergoing reconstruction after limb loss or loss of a body part after trauma. The first is osseointegration (OI) and the second is targeted muscle reinnervation (TMR) surgery.
These two surgical techniques are so important that they need to be described in a little more detail:
Osseointegration
Osseointegration is a biological phenomenon that describes how a titanium metal implant can be inserted into living bone and (over a 6-week period) becomes chemically bonded to that bone. The bond between the metal surface and the implant is so strong that removing the implant can be very, very difficult. This allows the metal implant to be used as a “bone-anchor” to allow direct skeletal fixation of a prosthesis to the residual skeleton in the amputation stump of a patient.
The bond also allows vibrations from the prosthesis to be detected through the bone (a process called osseoperception) that allows patients to detect the texture and consistency of the surfaces on which they walk or to be able to know where their prosthesis is in space, even with their eyes shut.
OI makes it possible to restore the correct biomechanics of walking for lower limb amputees instead of relying on a socket to carry the weight of the patient’s body. As a result, the energy of walking is reduced and walking gait can be improved if not normalised, especially for below knee amputees. OI is now considered as a well-established, and well-understood surgical technique although the availability of the surgical expertise required to make it work remains limited.
Targeted Muscle Reinnervation
Targeted muscle reinnervation (TMR) is a surgical technique for re-directing the nerve impulses in the amputation stump of a patient, with the intention of treating nerve-related pain and to improve the ability of a patient to control a prosthesis (especially for the upper limb).
The technique requires detailed knowledge of the anatomy of the residual limb and the functions of the residual muscles in the stump. Since the original trauma can result in significant distortion of the normal function and anatomy of the residual limb, it is often necessary to obtain detailed pre-operative CT-scans and electromyographic (EMG) studies.
At surgery, the nerve stumps are dissected free and can then be directed into redundant muscles in the stump which converts the muscles into biological amplifiers of the electrical signals in the nerve stumps.
When the muscles contract, the electrical activity is detected by electrodes placed on the skin and these can then be used to instruct a myoelectric prosthetic device to move. The electrical activity also results in feedback for the peripheral and central nervous systems which is effective for treating neuroma (NP = neuroma pain) and phantom limb pain (PLP).
TMR is now considered as a well-established technique for dealing with nerve -related pain although the availability of the surgical expertise required to make it work remains limited.
Although the emphasis of this article has been on possible solutions for amputees using OI and/or TMR surgery, patients, solicitors, and case managers should also be aware that the Relimb service can provide a complete range of reconstructive surgical options. Therefore, we strongly recommend that you consider getting in touch with the Relimb service whenever the thought arises that your client may need any form of reconstruction since it is likely that we will be able to provide them with a solution.

About Norbert Kang
Consultant Plastic Surgeon and co-founder of ReLimb
Read more insights into limb loss
View more articles related to Amputation and Team Around the Client








